Diabetes is a chronic metabolic disease characterized by a lack of insulin resulting in elevated blood glucose levels. Individuals with a fasting blood glucose level greater than 125 mg/dl are deemed diabetic. Diabetes has been linked with the onset of other chronic diseases including, but not limited to, microvascular complications, atherosclerosis, peripheral vascular disease, peripheral neuropathies, heart attack and stroke. It is one of the major risk factors associated with coronary artery disease.
Type I diabetes mellitus have an absolute deficiency of insulin resulting from dysfunction in the insulin-producing beta cells in the pancreas. As such, insulin must be supplied via injection or insulin pump. The onset of individuals with type I diabetes usually occurs prior to age 30 but can occur at any age. There appears to be a genetic link to an autoimmune response affecting the beta cells in the pancreas, ultimately leading to their destruction. Approximately 5-10% of the estimated 20 million people with diabetes in the United States have type I diabetes.
Type II diabetes mellitus have a relative deficiency of insulin. They can have elevated, normal or reduced insulin levels. These individuals are hyperglycemic regardless of their blood insulin levels. There are a number of proposed factors that lead to type II diabetes including a genetic link, environmental components, insulin abnormalities, increased glucose production in the liver, increased fat breakdown and defective hormonal secretions in the intestines.
Type II diabetes is characterized by peripheral tissue insulin resistance and defective insulin secretion. Glucose does not readily enter insulin-sensitive tissues (muscles and adipose) when there is insulin resistance resulting in elevated blood glucose levels. This results in a signal to the beta cells in the pancreas to produce more insulin in an attempt to maintain normal blood glucose levels. Regrettably, this additional insulin is usually ineffective at lower blood glucose levels and may contribute to additional insulin resistance.
Obesity is one of the major contributors to the onset of type II diabetes. The onset is insidious with few symptoms resulting in a diagnosis only after another organ damage has occurred. It affects approximately 90-95% of diabetics, unfortunately, roughly 6.2 million go undetected. It is associated with older age, history of gestational diabetes, obesity, family history of diabetes and race or ethnicity. The ethnic groups more commonly affected by type II diabetes include African Americans, Hispanic-Latino Americans, American Indians and Alaskan Natives. Type II typically occurs after the age of forty but with increasing childhood obesity and inactivity, the rate is increasing in young adults and youth.
There are a number of beneficial effects from exercise for diabetics. Clearly, the most critical is the possible improvement in blood glucose control. Exercise should be a critical component, in combination with diet and medication, to improve glucose control in people with type II. Exercise is typically not considered a component for treating blood glucose levels in type I, but those individuals are encouraged to exercise for the cardiovascular benefits. In type II, exercise has been shown to lower insulin insensitivity and lower medication requirements. Exercise leads to a reduction in body fat. Weight loss increases insulin sensitivity and may decrease the amount of insulin or oral hypoglycemic medications needed. Exercise improves cardiovascular health, a known risk associated with diabetes. Lastly, exercise may lead to the prevention of type II diabtes.
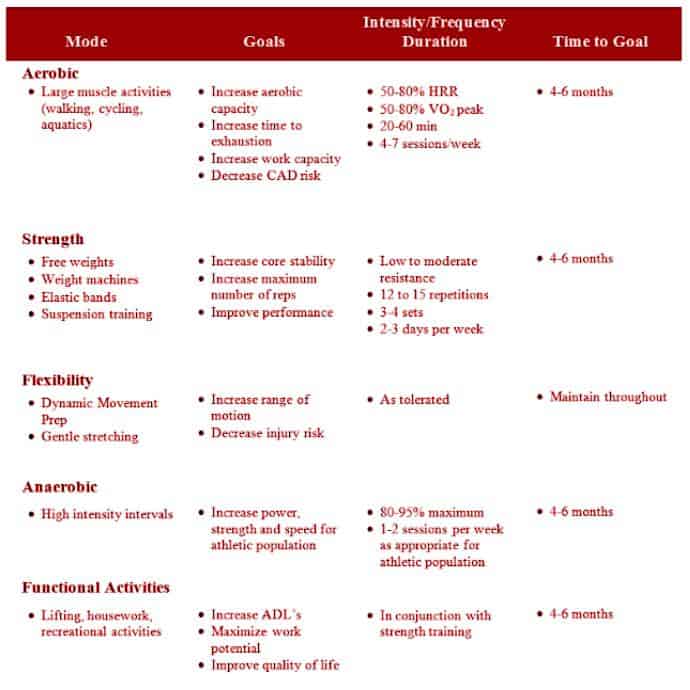
Exercise programs for diabetics must be individualized based on medication schedule, presence and severity of diabetic complications, client goals, and expected outcomes. There is no reason an individual with well-controlled diabetes cannot exercise, train and compete at any level of competition. Programs should be well rounded and include a component of endurance training, resistance training and flexibility, and balance. Specific considerations must be made for individuals on hypoglycemic medications. In general, one hour of exercise requires an additional 15 grams of carbohydrate either before or after exercise. People should consume an additional 15 to 30 grams of carbohydrate every hour during vigorous exercise longer than an hour.
Learn more about training Special Populations, including those with Hypertension, CAD, and Type I and Type II diabetes, in the Personal Fitness Trainer Certification Course.