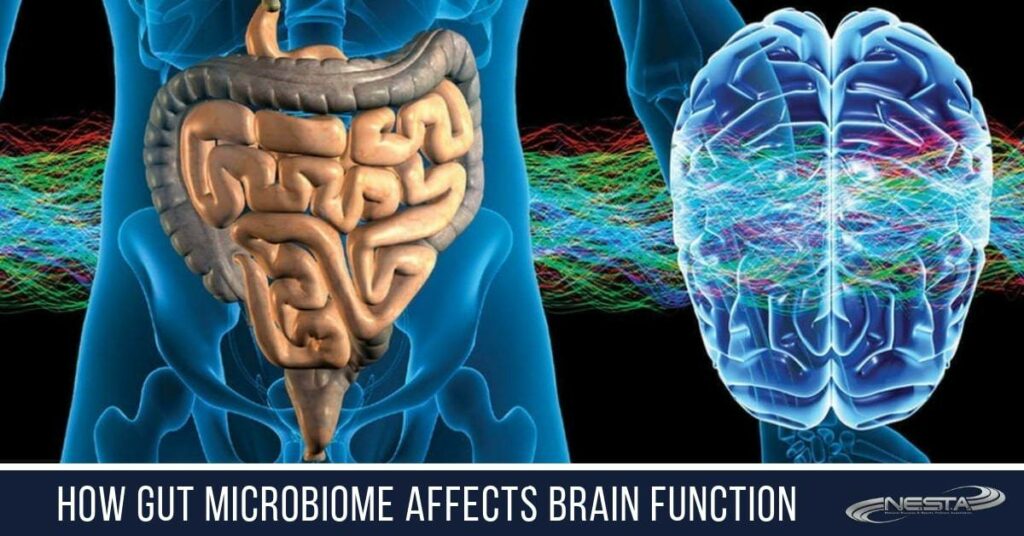
 Science is gradually discovering the secret of the gut feeling, as researchers have started to understand gut functioning better. Our Gut not only feeds the body and the brain (through absorption of nutrients), but it also has more neurons than the spinal cord.
Science is gradually discovering the secret of the gut feeling, as researchers have started to understand gut functioning better. Our Gut not only feeds the body and the brain (through absorption of nutrients), but it also has more neurons than the spinal cord.
The gut produces more serotonin and other similar neuropeptides than the brain or any other organs. Studies show that more than a trillion microbes reside in our body, weighing few kilograms, and the majority of them are in the gut. It seems that the role of gut is more than merely providing nutrients through digestion.
Whether you specialize in nutrition, health and wellness, sleep science, or brain fitness and function, understanding how our gut health affects the other aspects of our body and mind, and being able to relay that knowledge to your clients in a clear and succinct format so that they can improve gut health.
The Microbiome
These billion plus bacteria, fungi, and viruses colonizing our body are collectively called microbiota. And the collection of their genes is called the microbiome. Since the information found in microbiome exceeds hundreds of times the information found in human genes, microbiome must be playing some critical role in human existence.
There is another reason why there is an increasing interest in the microbiota, its role in health, and mental wellbeing. In the last few years, there has been an upsurge in non-communicable diseases like diabetes, hypertension, cancers, neurodegenerative disorders. Science knows that the human genome has not changed much in the last 50 to 100 years. But what has changed a lot is a lifestyle, diversity and quantity of microbiota, and thus microbiome. It could be one of the reasons why depression or Alzheimer’s have become one of the leading causes of mortality and morbidity, though just a century back, these conditions were classified as rare disorders.
Gut-Brain Axis and Microbiota
It is not only genes that are transferred from parents, but newborns are also exposed to mother’s microbiota during the process of birth, and it leaves its signature for the rest of the life. Studies show that microbiota plays an important role in brain development during the early years.
One the way researchers have learned the effect of microbiota on human health and brain development is by using germ-free animal models. Further, they also exposed these animals to various microbes found in the human body to understand their role in wellbeing. Using animal models may not be a perfect way to study the role of microbiota, but it still provides some necessary information.
There are several ways through which microbiota may modulate the gut-brain axis:
- The Vagus nerve– is a part of the autonomic nervous system. Researchers have long known how it helps regulate gut motility and functioning. For centuries, researchers looked at the vagal nerve as a pathway that starts from the brain and helps control the working of the gut. However, researchers were amazed to realize that Vagus nerve has more afferent fibers then efferent fibers. This means that Vagus nerve is providing a massive amount of information to the brain and is not merely there to control the gut activity. Therefore, researchers think that these sensory fibers in Vagus nerve influence the working of the hypothalamus and limbic system and thus modulating the emotions. It is now evident that the Vagus nerve is two-way traffic.
- Neuroendocrine signaling/gut hormone- in recent years researcher are starting to better understand the neurohormonal role of various organs – for years; they thought that it is the role limited to specialized endocrinal glands. However, now researchers know that gut lining produces many neuroactive substances like peptide YY, cholecystokinin, GLP-1 and 2, substance P, and many more. Gut microbiome not only influences the production of the neuroactive peptides but may also directly engage in their production. These hormones may have a direct influence on the enteric nervous system. These hormones are absorbed into the bloodstream and thus can influence the working of the brain.
- Interference with Tryptophan metabolism – it is a well-established fact, that serotonin (5-HT), a kind of neurotransmitter plays a vital role in mood regulation. That is why drugs used to treat mood disorders like depression work by interfering with the working of serotonin or its receptors. Researchers have discovered that almost 95% of serotonin is produced in the gut. In the gut, serotonin helps control its motility, secretions, and in the brain, it regulates mood and cognition. Gut microbiota plays an important role in the metabolism of tryptophan, an amino acid that is required to produce serotonin.
- Immune system- almost 70% of all the immune cells are related to the gut lymphoid system, which means that the biggest part of immune cells is concentrated in and around the gut. As most of the microbes also reside in the gut, they surely have a role in training the immune system.
- Intestinal permeability- low-grade inflammation and chronic stress affect intestinal permeability leading to the so-called leaky gut syndrome. It results in higher circulation of bacterial toxins in the blood, and other compounds. It is thought that leaky gut syndrome plays an essential role in the development of various mood disorders and diseases of the brain. Some studies seem to indicate that gut microbiota may have a role in mental disorders like depression, anxiety, autism, schizophrenia, and even in the development of neurodegenerative diseases.
- Microbial metabolites– some research indicates that microbial metabolites may affect the working of various body organs, including the brain. Some species of Lactobacillus may produce gamma-aminobutyric acid (GABA), an important inhibitory neurotransmitter in the brain. Similarly, species of Enterococcus, Escherichia, Candida may produce serotonin. Microbes may also provide various short-chain fatty acids like butyric acid or propionic acid thus stimulating the sympathetic nervous system, influencing the release of other neurotransmitters which may finally affect the learning processes, memory, mood, and much more.
Most brain or mental disorders develop gradually and over the years. Disease like Alzheimer’s may take decades to develop, and the same is right for depression in most of the cases. Therefore, researchers think that disturbances in gut microflora/microbiota may have something to do with these conditions. Evidence is emerging that gut microflora may influence the working of the brain in numerous ways. Moreover, studies are showing that these microbes can even produce some of the neurotransmitters. Further, microbiome or genes of these microbes may also interact with the working of the brain.
Major Depression and Microbiota
There is lots of research that shows the strong association between depression and gut microbiota. In many experiments, researchers have used animal models, and they were able to induce depression by altering the gut microflora, and some changes helped rescue these animals.
How these mood changes are happening due to gut microbiota is partially understood like these microbes can produce neuroactive compounds like serotonin, GABA, dopamine and thus may have a direct influence on the working of the brain. Further, these neuroactive compounds also modulate working of the intestine and affect the local microflora.
Autism Spectrum disorder (ASD) and Microbiome
Autism spectrum disorder (ASD) is a group of neurodevelopmental disorder characterized by poor cognition, poor communication skills, behavior issues, restricted social interaction, and so on. Researchers think that ASD occurs due to genetics, environmental factors, and other health problems during early childhood.
New research indicates the role of gut microbiota in the development of ASD. Microbiota may influence brain development through its role in homeostasis, amino acid metabolism, glutathione metabolism, affect immune responses, and so on. Those living with ASD are also at higher risk of other mental disorders. Gastrointestinal problems are more frequent in those living with psychiatric disorders. Various painful gut conditions like Crohn’s disease have a higher prevalence in children living with ASD.
Researchers have also found a correlation between the prevalence of ASD and the presence of certain bacteria in the gut flora like Clostridium or Desulfovibrio. Interestingly, some anecdotal reports show that by eradicating these bacteria with the help of antibiotics may reduce the symptoms of ASD in some children. Similarly, probiotics may also help by altering gut flora.
Researchers have also found some disbalances in gut microflora to be more common among the children living with ASD. Like the lower population of Coprococcus and Prevotella species.
Therefore, changes in gut microbiota or dysbiosis could be one of the contributing factors to the development of ASD.
Schizophrenia and But Microbiota
Schizophrenia is one of the most severe mental disorders that affect about 0.5 to 1% of the population. It is a condition that is characterized by delusions and hallucinations. A person living with the disease may believe in things that do not exist. It is one of the common reasons for admission to the psychiatric clinic. There are numerous drugs to treat the condition, but they can control symptoms only in a small number of patients.
New research seems to indicate that gut microbes may have a lot to do with the pathogenesis of the condition. Thus, studies show that those living with schizophrenia may have a higher population of certain microbes that increase the levels of gut lactic acid. Further, some of the bacteria may alter Th2 immune responses, commonly found in schizophrenia patients.
In a small number of cases, treatment with probiotics may help reduce the severity of symptoms.
One of the recent papers published in 2019 regarding the role of gut microbiota in schizophrenia found many interesting facts:
- Those living with schizophrenia had lower microbial diversity.
- Certain bacteria like Prevotellaceae, Veillonellaceae, Coriobacteriaceae, and Bacteroidaceae were more common in schizophrenia patients or in those who poorly responded to medications.
- At the same time, bacteria like Enterobacteriaceae, Norank, Ruminococcaceae, and Lachnospiraceae were in fewer numbers in schizophrenia patients.
- There were some similarities in microbiota changes in schizophrenia patients and those living with depression.
- The study was able to successfully differentiate between the patients with schizophrenia and healthy controls based on the analysis or gut microbiota (presence or absence of certain bacteria).
- The same study also tried to improve symptoms of mental disorders in mice with the help of fecal microbiota transplantation with some positive results.
Alzheimer’s Disease and Microbiota
Incidence and prevalence of Alzheimer’s are rising fast, and yet more than a century of research into the condition has failed to prevent or treat the disease. It is already one of the leading causes of death in some nations. At present, no pharmacological drug can considerably change the course of the disease. Researchers know that the accumulation of amyloid beta proteins in neurons and ensuing cellular death has lots to do with the disease development. But they do not know what causes the accumulation of amyloid protein in cells and how to stop such a buildup.
The latest research shows that gut microbiota may have lots to do with disease development. One theory is that altered gut microbiota may cause leaky gut syndrome, chronic inflammation, altered immune responses leading to the increased permeability of blood-brain barrier, neural injury, and neurodegeneration.
Researchers have also found that amyloid proteins are used by an innate immune response to fight certain infections. They still do not know the importance of the finding, but they think that it could be another clue how dysbiosis may have a role in disease development.
Manipulating the Gut Microbiota for Better Health
There are many ways in which gut microbiota can be altered; one of the most popular approaches is to use probiotics. Antibiotics, on the other hand, seem to have a negative effect on the gut flora as they may kill the beneficial bacteria, thus resulting in the overgrowth of harmful bacteria.
Diet also has a direct impact on the gut microflora. It could explain why certain kind of diets is better for brain health.
Neurological and mental disorders are quite complex. Modern drug therapy can barely control the symptoms of various such conditions and can rarely modify the course of the disease. More than a hundred years of research in certain disease conditions like Alzheimer’s, depression, has failed to produce results, improve understanding of disease process, or find a treatment. It is possible that a lack of knowledge about the role of gut bacteria in these conditions could be the missing link. At present, understanding of microbiota and microbiome is limited, but initial results show that their role is critical in wellbeing.
How You Can Help
If you want to help clients with food, diet, weight management and improving the results of their fitness routines, the Fitness Nutrition Coach course is for you. You will learn about optimal nutrition, including proven techniques for increasing energy, optimal health and decreased dependence on medications. Instantly increase your job and career opportunities with this popular professional credential.
Become a leading authority on brain optimization through proper training, sleep, nutrition, neuro-conditioning and flow state. As a Brain Fitness Coach, you know how important things like mindset, focus, clarity, determination, distraction control and flow are to success: mental, physical or financial.
When you become a Certified Sleep Science Coach, you will learn how to help your clients dramatically enhance their metabolism, memory, creativity, immune function, hormone balance, hunger management, disease prevention, sports performance, accident avoidance, memory, reaction time, good judgement, surgery recovery, happiness and over 100 additional functions and behaviors.
Check out what it takes to start a career in personal fitness training. This is your most affordable and fastest way to become a highly qualified personal trainer.
NESTA coaching programs are open to anyone with a desire to learn and help others. There are no prerequisites.
That’s it for now.
Take action!
PS: Click here to see many helpful business/career resources